Bed Sores – Decubitus Ulcers – Pressure Sores Stage 4 Four
Pressure Wounds are virtually always preventable and treatable. First you must clean the skin. You must reposition at least every 2 hours or more frequently and you must keep weight off the wound: Never sit on or lay on top of a pressure wound or it will not heal. Particular care has to be taken for signs of infection such as a strong foul odor and or large purulent (pus) drainage.
There are several stages of Decubitus Ulcers with stage 4 being the most serious/advanced. Pressure Sore Death can occur if a stage 4 bed sore decubitis ulcer is allowed to advance to infection and aggressive treatment is not successful. Most pressure sores are easily preventable. Our attorneys can review your nursing home medical records to determine if the nursing home has acted negligently in treating pressure sores.
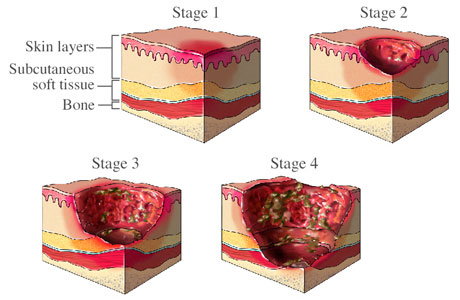
Pressure Sore Stages
The Federal Government has issued regulations that basically require nursing homes NOT to allow a resident who enters a facility to acquire pressure ulcers while under their care:
§483.25(c) Pressure Sores (also called Tag F314):
Based on the Comprehensive Assessment of a resident, the facility must ensure that-
(1) A resident who enters the facility without pressure sores does not develop pressure sores unless the individual’s clinical condition demonstrates that they were unavoidable; and (2) A resident having pressure sores receives necessary treatment and services to promote healing, prevent infection and prevent new sores from developing.
The National Pressure Ulcer Advisory Panel (NPUA) has published their definitions of Pressure Ulcers (updated in 2007):
Pressure Ulcer Definition
A pressure ulcer is localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear and/or friction.
Pressure Ulcer Stages
Stage I:
Intact skin with non-blanchable redness of a localized area usually over a bony prominence. Darkly pigmented skin may not have visible blanching; its color may differ from the surrounding area.
Stage II:
Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough. May also present as an intact or open/ruptured serum-filled blister.
Stage III:
Full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscle are not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining and tunneling.
Stage IV:
Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often include undermining and tunneling.
The Federal regulations and guidelines list the classic risk factors for bed sores –
- Impaired or decreased mobility and decreased functional ability
- conditions such as end-stage renal disease, thyroid disease, or diabetes mellitus
- Cognitive impairment
- Exposure of skin to urinary and fecal incontinence
- Under-nutrition, malnutrition, and hydration deficits
- recurrence of prior ulcer
Assessment Tools: Both the Braden and Norton scales help to measure Pressure sore risks.
Interventions such as frequent repositioning are critical in preventing pressure ulcers as well as treating ulcers.
Our Boston area Law office represents victims of Nursing home Abuse and Neglect. If your loved one has been injured or died as a result of nursing home abuse or neglect please call our Massachusetts attorneys at 1-617-479-4300

Hamill Clients win two more nursing home abuse verdicts
Nursing Home Links – and Resources
Pressure Sore Investigative Tool
Nursing Home Patient Rights
Investigate Your Nursing Home
Patients rights